One in every 200 people suffers from lymphoedema. Given that lymphoedema is such a common side effect of cancer treatment and several other conditions, why is it that most health care professionals don’t know anything about it?
What is Lymphoedema?
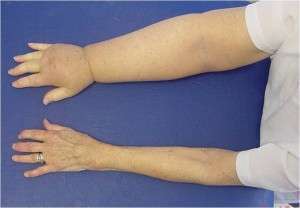
Lymphoedema is a build-up of protein rich fluid, resulting in swelling of the affected area. While it is most commonly seen in the limbs, it can also occur in the trunk, breasts, head and neck or genitals.
Until recently lymphoedema was categorised as a dermatological condition by World Health Organisation; however, it actually has little to do with the skin. The lymphatic system is a delicate network of vessels and nodes which lie directly underneath the skin. Vessels collect fluid from collectors and transport it to nodes which are situated in various areas in the body, e.g. in the armpit, behind the knee, in the groin and deep in the abdominal cavity where the main lymphatic duct is situated. The nodes act as transport hubs where the fluid collects before draining off to the next pathway of vessels.
The onset of oedema is due to an inability of the lymphatic system to process fluid, either due to an increase in lymphatic load or a decreased ability of the lymphatic system to function. If nodes are removed (as is common in cancer treatment) or the system is damaged, congestion occurs, like a traffic jam, and fluid needs to find a detour – but often is unable to.
While it is unfortunately an incurable condition, lymphoedema can be controlled with proper management. Many health care practitioners aren’t experienced in the diagnosis or treatment of lymphoedema (some have been known to tell patients they simply need to lose weight, which is understandably quite frustrating and upsetting for many!), so patients should try to find someone who has knowledge of the field. This is especially important because the longer lymphoedema is left without intervention, the harder it is to treat.
Lymphoedema can be classified as either primary or secondary depending on its mechanism of onset.
Primary Lymphoedema
One in 6,000 births result in a congenital condition where the lymphatic vessels have not developed properly. This is more commonly seen in the lower limbs, and usually both sides are affected. Some patients never notice any symptoms or sometimes the swelling may be set off by an event, such as an episode of cellulitis or a mosquito bite. Primary lymphoedema has been shown to have a genetic link; many patients report a long history of family members having “chunky legs.”
Secondary Lymphoedema
Secondary lymphoedema occurs due to damage to the lymphatic system either by surgery, infection, infiltration of cancer into the lymph nodes, or obstruction. The most well-known cause is due to axillary lymph node clearance for the treatment of breast cancer, however gynaecological cancers and resulting (pelvic and inguinal) lymph node clearances can often cause pelvic and lower limb lymphoedema as well.
Breast cancer surgeons now perform a Sentinel Lymph Node Biopsy, where they can remove one or two lymph nodes and assess if the cancer has metastasised. If there is disease in the sentinel node, then a full clearance will take place; however, if it is clear then the lymph nodes can be left. This procedure prevents healthy lymph nodes being removed unnecessarily.
The incidence of lymphoedema following a Sentinel Lymph Node Biopsy is 7% compared to 22% after a complete Axillary Node Clearance. Approximately 20% of all breast cancer patients will develop secondary lymphoedema as a result of treatment, with radiotherapy to the axilla and certain chemotherapy drugs also causing damage to the lymphatic system.
Other causes of secondary lymphoedema are damage to the venous system, dependency oedema (e.g., following heart failure), obesity and cardiac disease.
Lipoedema
It is also worth mentioning a condition called lipoedema, which can often be confused for lymphoedema. While lymphoedema is a build-up of swelling, lipoedema is an abnormal deposition of fatty tissue, usually seen in bilateral lower limbs and predominantly affecting women. It is thought there may be a hormonal link to lipoedema as some patients notice an onset of symptoms during pregnancy or menopause. If the excess fat cells place strain on the lymphatic system, it can lead to a build-up of oedema and a condition known as lipo-lymphoedema.
Preventing Lymphoedema
The easiest way to treat lymphoedema is to prevent it in the first place. Those identified as being at risk of developing lymphoedema should implement the habit of following limb precautions for the rest of their lives, as swelling can occur at any stage in the future.
The main rule of lymphoedema prevention is to limit the risk of infection in the limb where any lymph nodes have been removed.
Dos
- Keep limb clean and moisturised – dry skin is prone to cracking which provides a potential entry port for germs and bacteria which can cause infections
- Keep mobile
- Stay hydrated
- Wear gloves in the garden and while doing washing up
- Avoid extreme temperatures and sunburn by wearing long sleeves and sunscreen
- Avoid mosquito and insect bites by wearing repellent and long sleeves
- Take care when flying – there is no evidence of flying causing lymphoedema, however being immobile for long periods of time, dehydrated and lifting/pulling heavy suitcases can increase the load on the lymphatic system. It is advisable to be obtain compression garments before long haul flights.
Don’ts
- Any needles, injections or blood pressure taken from the affected limb
- Tattoos
- Undertake any repetitive heavy activity with affected limb
- Gain significant amounts of weight
- Wear tight clothes, bra straps, handbag straps that can restrict lymphatic flow
Cellulitis
The medical term for an infection of the skin and the underlying tissue, cellulitis is a lymphoedema patient’s worst nightmare. Each episode of cellulitis causes more damage to the lymphatic system. This then decreases its ability to process infection, resulting in being more prone to infections, quite the vicious cycle. If a patient has had multiple bouts of cellulitis, they should ask their GP for a prophylactic antibiotic prescription meaning they can go straight to the pharmacy and commence treatment at the first sign of infection. Recurrent episodes of cellulitis can result in hospital admissions and a dependency on antibiotics.
Diagnosis
Early warning signs of lymphoedema include heaviness, aching, watches / rings becoming tighter, and puffiness.
A qualified physiotherapist or other registered health care professional should conduct an observational assessment and ask the following questions:
- Is there visible swelling?
- Is it pitting? i.e., does the skin ‘indent’ when pressed?
- Any redness or skin changes?
- Can the wrist and elbow creases be seen (or the bones of the ankles if the lower limb is affected)?
Measurements
There are a few ways to measure and monitor lymphoedema:
- Circumferential measurements – These are commonly used; however, it is important to remember that they are not always accurate due to body composition. A patient’s limb circumference can increase due to fat or muscle gain, as well as an increase in fluid volume. It is always important to compare measurements to the other side of the body.
- Bio-impedance – This is a more accurate method. It is useful in picking up subclinical (early stage) lymphoedema and often used to gain a pre-operative bench mark.
- Perometry – This technique uses infrared light to measure the limb. The size and cost of this machine usually limits its usage to large specialist centres.
Investigations
A medical specialist may request one of the following investigations to assist with diagnosis:
- Doppler Ultrasound – This is typically used to exclude a Deep Vein Thrombosis (DVT).
- Lymphoscintigraphy – A green dye is injected into the lymphatic system in the web space either between the toes or fingers. The flow of the dye is then mapped out under fluorescent light and any obstructions or dysfunctions can be seen.
The Stages of Lymphoedema
Lymphoedema is described as progressing through the “Three Fs”
- Fluid
- Fat
- Fibrosis
Essentially, the swelling becomes more ‘solid’ as the condition progresses. As you might appreciate, it is much easier to treat and drain oedema that is in the fluid stage before it becomes firmer and harder to shift.
There are several different methods of staging lymphoedema. The most widely accepted is from the International Society of Lymphology
- Stage 0 – Subclinical oedema, no swelling is visible but may be picked up with bio-impedance
- Stage I – Early onset lymphoedema, swelling resolves with elevation
- Stage II – Elevation no longer helps reduce swelling and pitting is present, sometimes late in this stage, the swelling no longer pits as the fluid progresses to fat and later fibrosis
- Stage III – More commonly known as elephantitis, the limb can be very large with significant skin changes
Classification of Severity
In cases where only one side of the body is affected, the severity of lymphoedema is assessed by comparing the affected limb to the unaffected one:
- Mild: < 20% limb volume difference
- Moderate: 20 – 40% limb volume difference
- Severe: > 40% limb volume difference
Physiotherapy Treatment of Lymphoedema
Education
This is arguably the most important part of treatment and should start with preventative education for patients at high risk of developing lymphoedema. It needs to be emphasised to patients that the condition is progressive in nature and, if left untreated, it will worsen.
Treatment will depend on the severity of the oedema and can occur as either an intensive or maintenance phase. Patients with established oedema may experience flare ups but they should have several treatment techniques in their tool box to manage swelling independently or with the help of a physiotherapist.
Compression
Often the most effective way of reducing limb volume is through compression techniques. Compression can be achieved in several ways:
Bandaging
This is done by either Multi-Level Lymphoedema Bandaging (daily and heavy) or a newer technique using Coban, which is much lighter and can be redone every two days for best results.
Garments
Garments can be useful for providing graduated compression. The highest pressure is always placed towards the end of the limb, as it’s imperative fluid is not pushed away from the mid-section.
Garments can be constructed in flat knit or circular/round knit and be either off the shelf or custom made for more irregular limbs. They should be always be fitted by a physiotherapist initially to ensure the appropriate goals will be achieved.
Garments are usually worn all day and removed at night, but must be worn during exercise as the compression helps to facilitate the muscle pump. It is possible for patients to access assistive devices to help with donning/doffing of garments.
Wraps
Wraps are handy for night time use or as an alternative for patients who struggle with donning/doffing of garments due to mobility issues or arthritic fingers.
Intermittent Pneumatic Compression
A compression pump can be very useful for use at home or in clinics where resources are stretched. Pumps are generally not as effective as a therapist’s hands due to the generic compression cycle, but are still valuable replacements when required.
Manual Lymphatic Drainage / Self Lymphatic Drainage
This refers to a massage technique which attempts to encourage the oedema back into the central system for processing. The traditional Manual Lymphatic Drainage technique was incredibly gentle and a large amount of time was spent “preparing” the area of the body just above the swelling.
However, via fluoroscopy, the technique has been updated to a firmer pressure and there is now no need for proximal “preparation”. The new technique is known as Fluoroscopy Guided MLD. Patients are taught Self Lymphatic Drainage (SLD) by a physio and they can then use this as part of their daily management routine.
Skin Care
Skin needs to be kept clean and dry with care taken to prevent infections, cuts and scratches. Patients should moisturise daily, with the optimal time being at night after a shower to allow the moisturiser to sink into the skin while a compression garment is not being worn. Finger and toe nails should be kept short and clean to avoid any scratches.
Exercise
Exercise is one of the most important, but unfortunately often neglected, elements of lymphoedema treatment. During exercise, muscles naturally act in a pumping fashion to enhance lymphatic return. By wearing a compression garment while exercising, additional pressure can be applied to assist the pump. Exercises should generally be guided by a physiotherapist to avoid repetitive overload on the affected limb, as too high a load can place more strain on the system.
Lymphoedema patients need resistance exercises in their regime to increase lean muscle mass. If they experience significant weight loss, skin loses the elasticity which provides resistance to the swelling. Being overweight is a risk factor for developing lymphoedema, and patients who have established swelling should try to maintain a healthy weight to avoid placing more load on their already struggling lymphatic system.
It can be very difficult for lymphoedema patents to develop an effective fitness routine. They sometimes find it hard to mobilise, develop concerns with body image and gain weight, causing a further strain on the lymphatic system. This is another reason why physio guidance is crucial.
Other treatment modalities
Low Level Laser Therapy – There is currently insufficient evidence as to its efficacy, but it may be effective in treating fibrotic areas.
Kinesio taping – This may be useful on areas where compression garments and bandaging are impractical, e.g., the head, neck and truck.
Surgical interventions
As with most things, surgery is generally a last resort and patients should not consider surgery as a quick fix for lymphoedema. However, with surgical techniques always evolving, there are some procedures which may be considered when non-surgical treatments have been unsuccessful:
Lymph Node Transfer
This is typically performed in cases where a lymph node clearance has taken place. In this procedure, lymph nodes from an unaffected region are grafted and implanted into the cleared area. This procedure has mixed reviews amongst surgeons, since by removing lymph nodes from an unaffected area, there is an increased risk of a healthy limb developing lymphoedema.
Lymphovenous Anastomosis (LVA)
This micro-surgery, used in patients with mild to moderate lymphoedema, involves lymphatic vessels being connected to veins to bypass the damaged area and restore the lymphatic flow from the oedematous limb. This procedure shows good results in early stage lymphoedema where there have not been any skin and tissue changes and lymphatic vessels are still in working order.
Liposuction
For select patients only, liposuction is another alternative treatment. Importantly, it must be done by a specialised lymphatic plastic surgeon, not a cosmetic surgeon. Liposuction has the benefit of reducing the weight of the limb, decreasing pain and increasing comfort and mobility for the patient. Post-operatively, patients need to wear compression garments at all times to prevent the oedema returning.
Debulking
Now somewhat of an outdated procedure, debulking is where fibrotic and fatty tissues are removed to reduce the size of the limb and skin is grafted over the wound. Patients are left with a smaller limb with plenty of scar tissue, but the insufficient lymphatic system hasn’t been improved, therefore fluid can re-accumulate (in a more limited space). This surgery may be considered for advanced cases of lymphoedema; however the patient’s quality of life needs to be considered due to possible complications of this procedure.
Seek Assistance!
The most effective treatment methods for lymphoedema are the ones that the patient is compliant with and those which allow them the most independence in their daily life.
If you’re experiencing lymphoedema, ask around and try to find a GP and physiotherapist who are confident and experienced in the management of lymphoedema. Implementing the right strategies at the right time can make a world of difference.